The Joint Commission have stringent requirements in place to keep your patients, employees and visitors safe. One of those requirements and concerns as a healthcare facility manager is the ventilation in your care areas. A ventilation system is effective at reducing hospital infections.
HVAC systems are built to keep the indoor air quality (IAQ) safe for patients. Because of the airflow standards, equipment must meet high ventilation rates and filtration requirements.
Richard D. Hermans, PE, HFDP, Director of Training and Advanced Applications for Daikin Applied, cites certain aspects of ventilation have become commonly accepted practice for infection control.
"They include negative pressure in isolation rooms, positive pressure in operating rooms, positive pressure in protective environment rooms, and filtration requirements for all areas of the hospital."
[source: The evolution of health care ventilation]
What is Ventilation in a Healthcare Facility?
When we think of ventilation in general it is simply moving air from one location to another through duct work. Air is cleaned by filters and released into the space intended. When it comes to hospitals, we go a level deeper with specific rooms needing to be either positively or negatively pressurized with respect to adjacent areas.
The purpose of positive pressure is to ensure airborne pathogens do not contaminate a patient or equipment and supplies in that room. So extra air is pumped into these rooms to push contaminates away from entering.
Negative pressure, sucking air out of the room, is used to pull any potential contaminants out of an area and exhaust them to the outside air. Negative room pressure is an isolation technique used in hospitals to prevent cross-contamination from room to room.
How much air is exhausted and how much air is supplied, the area is considered either negative, neutral or positive.- more air out, negative pressure
- same air in and out, neutral
- more air in, positive pressure
Ventilation Testing and Room Pressurization for Healthcare Facilities
As part of ventilation testing, rooms must be examined and documented to evaluate if further investigation is needed. Professional inspectors and HVAC specialists have equipment to measure relative pressures, volumes and air exchanges.
An example of a negative pressure room would be a patient with active Tuberculosis. The germs are "sucked out" of the room and exhausted, not spread around the hospital.
Conversely a patient with burns or open wounds would be in a positively pressurized room to discourage pathogens in the hospital from getting to the patient.
Pressure Relationship Within the Operating Rooms vs. Other Areas
Positively pressured rooms are typically considered the cleanest rooms in the hospital. Think of an OR that needs to protect the patient and all the sterile surgical supplies.
Due to patient vulnerability, operating rooms should have a positive pressure relationship to all adjacent areas.
"ASHRAE interpretation IC 170-2008-5 states that the OR should be positive to Sterile Storage."
Rooms may be positively pressured to protect patients, clean supplies, or equipment in a room. If these rooms are not pressurized properly, airborne contaminants from bordering areas may be pulled into them.
Managing Risk Associated with Utility Systems to Improve Performance
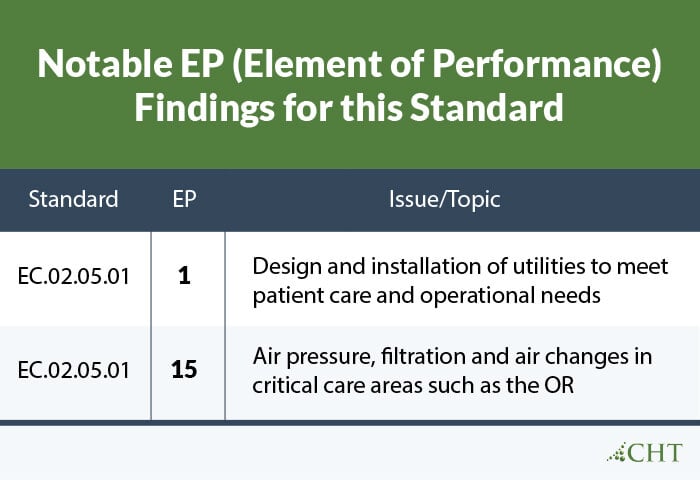
The Joint Commission continuously looks to improve standards and safeguard patients. The EC.02.05.01 Standard (The hospital manages risks associated with its utility systems), is just one of the standards to help healthcare organizations improve performance.
A life safety surveyor will note the deficiency if a marked room is not in compliance with TJC's standard (EC.02.05.01). An issue could be air pressure, filtration and air changes in critical areas such as the OR.
[source]
Here's an example from The Joint Commission of what improved compliance EP 1 and EP 15 would entail.
Issue:
Protect patients from airborne contaminates
Properly designed and installed ventilation systems reduces the concentration of airborne contaminates through dilution, filtration, and pressurization.
Risk:
Hospital-acquired infections
Inability of the utility systems to operate as expected may result in air-borne contaminates negatively impacting an already compromised patient.
Impact:
Harm to the patient
Airborne contaminates are a significant source of health care-associated infections (HAI). HAI may adversely impact patient during a hospital stay.
Mitigation:
Ensure utilities equipment effectively meets clinical needs
Properly designed, installed and maintained ventilation systems contribute to the reduction of HAI. Environmental controls will create a compliant patient care setting resulting in high reliability.
Infection Control and Prevention Through Ventilation
"Standard 170-2017 considers the chemical, physical, and biological contaminants that can affect the delivery of medical care to and the convalescence of patients, as well as the safety of patients, health care workers, and visitors."
source: ANSI/ASHRAE/ASHE Standard 170-2017: Ventilation of Healthcare Facilities
Infection control and prevention identifies and separates patients who are accessible and gives them extra protection.
According to HPAC Engineering, Standard 170 provides additional information in terms of minimum outdoor air changes and total air changes required for each type of space along with which spaces are required to be fully exhausted.
Conclusion
Controlling your air flow will benefit your patients, employees and visitors. It will also keep you compliant with The Joint Commission. There are safety measures to be taken in order to provide a safe environment.
CHT can provide pressure and air flow tests with documentation as part of your Vitaleyez program profile that satisfies the code. CHT inspectors and verifiers speak TJC, CMS, NFPA99-2102, ASSE, OSHA, FGI and several other languages to help everyone breath easier.
They can assist in making sure your rooms are appropriately pressurized and you will not get cited for EC.02.05.01.




