Most people think of the medical gas system as a pipe that pumps oxygen to patients in surgery or into their hospital room. In fact, there are several gases that make up the average medical gas system, including the anesthesia gases that are part of the cart in the operating room.
Medical gas systems sustain life and the gases they contain are regulated as a drug. Using medical gas systems properly includes navigating multiple layers of restrictions and instruction on the proper, safe and legal way to do things.
According to CBC News, the first recorded medical gas cross-connection deaths were at a former Sudbury General Hospital in Canada back in 1973. Codes were implemented to prevent future medical gas-related deaths requiring third-party verification and system installation certification.
The concern for patients and the efficiency of hospitals has led to several layers of oversight of medical gas systems from the government (CMS and OSHA), their agents (TJC and NPV), and the industry in the NFPA 99-2012 code. While all these organizations have oversight and regulatory power over medical sites using gases, their regulations often need to be more consistent.
Since there is so much scrutiny concerning medicinal gas systems, most hospitals hire third-party inspectors annually to check every element of their system.
A third-party inspector confirms that the medical gas systems are functional and meet the standards set by the organizations above, ensuring the safety of patients and staff. Not passing a medical gas inspection (or receiving citations) can affect a hospital’s reimbursement and/or accreditation status.
This guide provides an overview of medical gas systems, including
- Medical Gas Source Equipment
- Manifold Rooms and Equipment
- Medical Gas Alarm Systems
- Patient Room Gas Connections
- Hoses, Pigtails, and Connectors
- Additional Resources
Are you struggling with Medical Gas Compliance?
CHT offers medical gas services to help you reach your compliance goals. To help you navigate through these challenges, start with a free 30-minute discovery call.

![]()
Chapters
Chapter 1
Medical Gas Source Equipment
Piped medical gas comes from somewhere, and like running water, you don’t think about it until you open the faucet and nothing comes out. Source equipment includes the pumps, compressors, manifolds, and bulk containers that provide or create medical gases in the hospital piping system.
Source equipment may have multiple pieces of hardware to filter, pressurize, clean, dry, or regulate the gas to provide a clean and safe pressurized medical gas that meets the NFPA-required pressure and volume rates at each medical gas terminal.
Let’s first consider the most popular medical gas, Oxygen.
Oxygen
Oxygen can come from a high-pressure cylinder and, in some cases, like dentist offices, may, in fact, be connected directly to the equipment that touches the patient. Most hospitals and even medical buildings have an oxygen supply that comes from a tank of liquid oxygen stored in a specialized location. This tank is often stored outside the building.
Commonly, in the back of the hospital, you will see a very tall white tank connected to pipes at the bottom and surrounded by a fence. This tank contains hundreds of gallons of liquid oxygen. A hospital is required to have a minimum of one day’s supply on hand and a backup supply of one normal day should the main system fail to sustain patients, giving them time to fix or replace the primary oxygen supply.
The liquid oxygen boils at normal temperatures, and the gaseous phase is piped at a regulated pressure into the hospital building. The oxygen, still in a gaseous phase, is measured, and pressure is regulated before being piped throughout the building. It is important to note that there must be a shut-off valve and a pressure-sensing alarm at the entry point.
In fact, the main and backup oxygen sources are monitored so that systems monitoring the primary and backup supply can tell how much gas is present and if it is at the correct pressure. This information is presented to the facility manager on a Master Alarm panel as well as the duplicate master alarm panel often found in the security offices. Supply and pressure levels are monitored 24/7.
Cylinders of oxygen are identifiable by their color (green), label, and unique gas-specific connection fitting. They may be connected to a manifold and then to a master alarm and control valves and gauges. Some organizations use small tanks of liquid oxygen, commonly referred to as dewars or cyros, that function similarly to large outdoor tanks but can be inside the building in a specialized room. (See manifold rooms below)
Once the oxygen is in the piped gas system, it follows through a special copper pipe that has to be brazed together in a nitrogen atmosphere. These oxygen pipes in the walls and ceilings of the hospital deliver pure oxygen to the outlets on the wall we are used to seeing. Before the oxygen gets to those outlets, it is valved, gauged, and alarmed one or two more times.
The system is set up to be able to isolate a section of the hospital piping for repair, maintenance, and inspection purposes. Zone valves are accessible and located on the patient floors to isolate a group of patient rooms in the event of an emergency or maintenance. Some zone valves will have a zone alarm panel located on the same floor to monitor the pressure that is delivered to each terminal.
These valves must have visual gauges attached downstream of the valve to give a visual reading of the pressure so that hospital personnel will know the pressure in the line. Zone valves and gauges are often built into a box set into the wall so that only authorized people can touch them.
The oxygen flows from the zone valve to outlets in patient areas or another local alarm and valve setup near, but not in, the operating or procedure rooms. The oxygen flow may then be connected to anesthesia equipment or a breathing mask.
The oxygen is distributed through the outlet on the wall with a gas specific “quick connect” type fitting that comes in 7 different mechanical configurations. Oxygen outlets, fittings, and flexible hoses are colored green and will only connect with oxygen components.
Patients connected to house oxygen will have a volume regulator usually connected to the wall outlet to control the amount of oxygen coming to their mask or canella. The pressure regulator will also function as an on/off valve for the gas coming out of the wall. Because these outlets are plugged and unplugged constantly, they are the biggest wear component of the system.
Medical Vacuum
Vacuum is the second most popular medical gas in use and is often seen by patients and visitors. The vacuum is created by running a mechanical pump like a compressor in many regards, but instead of creating a high pressure in the pump and sending that compressed gas to the receiver tank, this pump sucks the gases out of the receiver tank and forces the compressed air outside leaving a vacuum in the receiving tank connected to the house piping.
Vacuum pumps come in several mechanical designs and must be redundant. Since they may be running 24/7 under varying loads, they will have various controls and alarms to maintain the pressure and activate the second (or third) pump if needed.
In some cases, the running of these pumps alternates to provide equal wear. The vacuum pressure is metered and sent to the master alarms. Commonly, zone valve boxes will have a vacuum line valve, gauge, and perhaps a sensor inside, along with the oxygen equipment. Depending on the setup, there may be other pipes, valves, gauges, and sensors for additional gases in the zone box.
Inlets connect the patient-area vacuum with the same gas-specific quick-connect setup as the oxygen. Each gas has a unique hose connection. Therefore, you cannot plug a vacuum device into an oxygen outlet or any other outlet.
These unique fittings protect against cross connections where equipment mishandling could inadvertently send the wrong gas to the patient. The vacuum inlets and connectors are white. In most cases, patient use of vacuum systems is done using a regulator plugged into the wall inlet. The regulator displays the strength of the vacuum and acts as the on/off valve at the site.
One of the challenges of maintaining a vacuum is that, in actual use, it draws fluids and solids out of bodies to make surgery and breathing easier. Inherently, this means “gunk” of many kinds and consistencies is pulled into the plumbing. In surgery, gravity traps called canisters capture most liquids and solids but cannot stop the aerosolized matter.
At the point of use, these fine particles are hardly visible. Still, as the material gets pulled through the system, it may accumulate inside the piping, even getting into receiving tank and the pump itself. Matter accumulation is often a problem in surgery, where the greatest amount of matter is suctioned. The lines from the inlets and even the plumbing in the operating room can occlude, reducing the volume and pressure the inlet can deliver to the surgical staff.
Typically, the remedy when this happened would be to replace the plumbing in the wall, which was expensive, time-consuming, and took the operating room and adjacent areas out of service. Today, CHT has developed a patented VacWash machine that allows the surgical vacuum system to be cleaned during off hours without replacing any inlets or plumbing.
Waste Anesthetic Gas Disposal
The Waste Anesthetic Gas Disposal (WAGD) system is also considered a medical gas system, though it is a unique vacuum system designed for surgery or procedure areas. Anesthesia gases heavily sedate patients during surgery. An anesthesiologist achieves the right combination of patient sedation while maintaining breathing by mixing the anesthetic gas with nitrous and oxygen.
This is very tricky and requires the doctor to monitor respiration and heart rate very closely while administering gases to the patient breathing mask or equipment. Not all these gases are consumed by the patient. In fact, with every exhale, the patient returns some of the anesthesia to the mask. Exposure of even small amounts of these anesthesia gases over a long period of time can be harmful to the staff doing the surgery, so the WAGD system uses vacuum pumps to draw the excess and exhaled gases away from the patient, the anesthesiologist, and the others in the operating room.
Depending on the volume of surgeries performed, the WAGD system may be plumbed completely separately from the vacuum system or merged with the general vacuum piping at some point outside the operating room. The focus is to draw away these excess gases and pump them outside the building, usually through a roof vent placed away from people and other air intakes.
WAGD inlets, tubing, and piping will be labeled and colored purple. The fittings for WAGD are gas-specific and cannot be connected to any other outlet or inlet. The vacuum pumps for the WAGD system are inspected like the other mechanical equipment in the source equipment room. The main concern for the WAGD system is that the vacuum pressure is maintained at a strong enough level to pull the flammable mixture of anesthesia, nitrous, and oxygen through the system and out of the building before it can ignite.
Medical Air
Medical air is the only gas manufactured on-site and delivered to the patient for breathing purposes. Medical air is a prescribed drug by a doctor, and because of that, the air quality of the gas must meet the United States Pharmacopeia (USP) requirements. Medical air is created centrally to provide a reliable supply of breathing air with the right humidity. Medical air is drawn from outside air using an intake vent away from other gas activity and pulled into a compressor to its boost pressure. The compressed air is then sent through an aftercooler to the receiver tank. On the way to the receiver tank, the medical air goes through a drier that removes moisture that accumulated during the compression process. The medical air passes through a “dew point” sensor that adjusts how much the drier has to do to make air comfortable for breathing. There is likewise a sensor in the medical airline to check for Carbon Monoxide, which could be fatal if administered during surgery. During use, the medical air comes from the receiver tank through a one micron filter and past a test port. The medical air flows into the house system through a valve, sensor, alarm, and mechanical gauge in the source equipment room. Medical air fittings are colored yellow and will only fit medical air outlets.
Like vacuum, medical air must be available 24/7, so the compressor has to have at least one redundant partner. These pumps are typically inspected every three months or 300 running hours. The preventative maintenance inspector measures electrical inputs to diagnose any internal friction in the pump and visually inspects belts, driveline parts, and the sensors in and around the pump to ensure it sends the proper signals to the alarms.
A compressed air dryer is used to remove water vapor from compressed air. Redundant compressed air dryers are mandatory for medical usage. The process of air compression concentrates atmospheric contaminants, including water vapor. This raises the dew point of the compressed air relative to free atmospheric air and leads to condensation within pipes as the compressed air cools downstream of the compressor. Excessive water in compressed air, in either the liquid or vapor phase, can cause operational problems for users of compressed air, especially breathing medical air.
The dryer’s performance is measured by the dew point or the amount of water in the air coming out of the dryer. Too much water in the air (a dew point that is too high) will trigger alarms. All driers require a drain to evacuate the water collected from the compressed air. These drains must be kept clear.
Desiccant Dryer
A regenerative desiccant dryer typically delivers a dew point of between −40 °F (−40 °C) and −100 °F (−73 °C). A refrigerated dryer provides a dew point not lower than approximately 32 (0 °C). A deliquescent dryer delivers a dew point suppression that fluctuates with air temperature. Typically, this suppression is 20 °F (11 °C) below the compressed air temperature.
In a desiccant dryer, compressed air passes through a pressure vessel with two "towers" filled with media such as activated alumina, silica gel, molecular sieve, and other desiccant material. This desiccant material attracts water from the compressed air via adsorption. As the water clings to the desiccant, the desiccant "bead" becomes saturated.
The desiccant dryer is programmed to switch towers based on a standard cycle time or amount of moisture accumulated. The dryer switches the flowing air to the second tower for drying. The first tower’s beads are purged by a blast of compressed air from the system, simply blowing off the water that has adhered to the desiccant. While the second tower collects moisture from the air flowing to the receiving tank, the water in the first tower is blown to a drain that opens at the bottom of the first tower. At the end of the cycle, determined by time or desiccant saturation, the system reverses so that the first tower resumes purifying and the second tower is blown dry.
The duty of the desiccant is to bring the dew point of the compressed air to a level in which the water will no longer condense or to remove as much water from the compressed air as possible. Many newer dryers come equipped with dew-dependent switching (DDS), allowing the dryer to detect dew point and shorten or lengthen the drying cycle to fulfill the required dew point. Often this will save significant amounts of energy, which is one of the largest factors when determining the proper compressed air system.
Smaller facilities may supply medical air in cylinders through a manifold or a regulator to the patient.
Instrument Air
Instrument air is similarly generated by compressors in the source equipment room. This compressed and filtered outside air is used to power equipment. The compressors and dryers in this circuit need to be inspected quarterly, like the medical air above. Medical air piping, fittings, and hoses are red, and their fittings are unique to that gas and its equipment. An instrument air dew point expected from a regenerative dryer is -40 degrees Celsius.
Source equipment rooms must be ventilated and maintained at a temperature that will allow the cooling mechanisms of the pumps to work well. Pumps that overheat trigger alarms and will shut down if the source equipment room air flow is not sufficient and does not maintain a safe equipment room temperature.
Chapter 2
Manifold Rooms
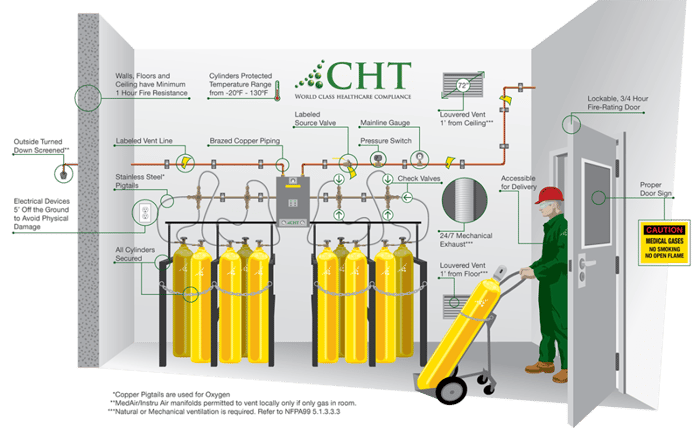
While vacuum, WAGD, Medical air, and Instrument air are generated locally in most hospitals, lower-volume gases may come through a piped system from cylinders connected to a manifold. Hospitals commonly have nitrogen, nitrous oxide, and carbon dioxide produced through a manifold.
The manifold room typically has various cylinders of different kinds of gas lined up against the walls. Cylinders contain very high pressure and must be protected with heavy-duty screw-on caps. These cylinders are supported (usually chained) in a vertical position. Some of the gas may liquify inside the cylinder, and the liquid can freeze the fittings, valves, and alarm sensors if it squirts through the pigtails (connecting lines). Keeping the cylinders vertical means compressed liquid will be at the bottom of the cylinder and not likely to foul the equipment. Each kind of gas will come in color-coded cylinders, plainly labeled with their contents name, and have unique connectors to ensure no cross-connection of gases. Labels must also state if a cylinder is empty or full.
Each kind of gas will be connected to the manifold through a “pigtail” or semi-flexible hose or tubing with the appropriate fittings to match the kind of gas being used. These pigtails must be the special copper tubing if a manifold supplies oxygen. Other gases will use reinforced rubber or plastic hoses. Usually, four or more cylinders connect at one time to the manifold, and each connection point has a one-way check valve so the cylinders can be changed without lowering the pressure of the whole system. The gas flowing from the cylinders goes to an alarm-equipped pressure regulator, where there is a mechanical valve to allow isolation of the system and a visible gauge before the gas goes into the house piping.
The infographic below shows most of the requirements for a manifold room as described by NFPA 99-2012.
Chapter 3
Medical Gas Alarm Systems
Medical gas alarm systems can vary in what they report and measure. NFPA and agencies set the minimum standards, but with current technologies, many alarm panels display more than the minimum requirements. Medical gas alarm panels come in three general descriptions or levels of protection:
- Master alarm panels that monitor source equipment, manifolds, and main oxygen supply.
- Zone alarms that will protect a section of the hospital and typically monitor the presence and pressure of oxygen.
- Area alarms that monitor oxygen and vacuum in the surgical, procedure, and recovery rooms. Critical care and anesthetizing locations are required to have area alarms to monitor each type of gas. Newer sensors and digital internal components can display various pressures and other measurements directly on the alarm screen.
Each alarm is associated with a valve and visual gauge to allow for the isolation of different parts of the system for emergency or maintenance purposes. Wireless signals can connect modern alarms to the sensors and other alarm panels. This method has many restrictions and safety requirements to avoid radio frequency interference and hacking.
Each pipeline coming to the valve is equipped with some sort of sensor. The type of sensor will determine what values are measured. The presence of the required gas and the pressure it supplies are determined. That information is sent to the alarm panel. The alarm is required to show a light or signal when the pressure is not correct and sound an audible alarm. Alarms can be silenced to reduce stress but will sound again when another signal is activated. Some alarms can be programmed to resume sounding if the out-of-spec condition continues.
Master Alarm panels should be installed in multiple locations. One should be located in an area of responsible surveillance, like the facility’s office or engineering office, and one should be located in an area with 24/7 surveillance, like a security office. If there is a break in the supply of these life-saving gasses, the alarm must warn everyone.
For most hospitals with cryogenic oxygen in an outdoor tank farm, the master alarm will have lights to show:
Oxygen:
- High main line pressure
- Low main line pressure
- Primary liquid level low (Less than an average day’s supply)
- Reserve in use
- Reserve liquid level low (Less than an average day’s supply)
- Reserve low pressure
- Manifolds with dewars or cylinders (Usually Nitrogen, Nitrous, CO2)
- High main line pressure
- Low main line pressure
- Secondary in use (changeover)
- Reserve in use
- Reserve low pressure
Medical Air:
- High main line pressure
- Low main line pressure
- High dew point
- Carbon monoxide level*
- High temperature* (Operating temperature of the compressor)
- Lag*
- If using liquid ring compressors, there must also be a high water gauge in the tank
- LPM* & high water in the separator
Vacuum:
- Low vacuum pressure
- Lag*
Instrument Air:
- High main line pressure
- Low main line pressure
- High dew point
- High temperature at compressor*
- Lag*
*The master alarm may display these signals under a common error code like “Maintenance required.”
The number of lights and the arrangement can vary depending on the details of the source equipment being used. Some types of pumps require extra alarms and some backup systems will also require alerting the 24/7 station. The emergency backup supply circuit must power alarms, so they work even if outside power is interrupted.
Where there are multiple sources, perhaps in various buildings, these sources will also need to be identified on a master alarm. In those cases, facilities should be told which system is alarming as well as the symptom.
The most crucial action to be taken by the person that monitors a master alarm is to ensure maintenance is called immediately to look into any alarm sounding. Informing the correct person about changes in alarm displays can save lives. Acting quickly and efficiently can ensure that life-sustaining medical gas continues to flow.
Annual and CMS inspections will go over the panel to confirm the correct signals are available and that all lights are working. While not part of a regular inspection, the sensors on the pipeline can and should be tested.
JC and CMS also require that the facility demonstrate reporting that the alarms are not only there, but they are properly monitoring the equipment and activating the proper alarms. NFPA and ASSE require alarm sensors and switches to be tested to ensure the functionality of the signals. Since these tests may interrupt the gas flow, they are done with advance warning by certified experts.
The zone alarm typically covers a floor or part of a floor of patient rooms. Likewise, it alerts if the supply drops for some reason with lights and sound.
The area alarm is placed close to, but not in, the same room as the gases being used to allow people outside the operating rooms to attend to alarms and the associated valve and gauge inside the wall box.
Chapter 4
Patient Room Gas Connections
In most modern hospital rooms, there are at least duplicate sets of oxygen outlets and vacuum inlets. This redundancy allows for continuous functioning in case of blockage or breakdown and may allow multiple devices to be used on patients.
Both connections are of the “gas-specific quick connect" type. That is, they are spring-loaded to turn off the gas supply when nothing is plugged into them. Most often, the wall outlet will have a regulator of some kind plugged into it, which allows the amount of oxygen or vacuum to be adjusted to fit the patient or machine’s needs.
The regulator will display the operating volume (the amount of gas flowing is adjusted by the staff). The regulator will function as the on/off switch for the gas connected to it.
Because these outlets are frequently used, they tend to wear out faster than other medical gas equipment. Outlets are plugged and unplugged often and may be replaced more regularly than other medical gas system components.
There are seven (or so) designs for the connectors and inlets designed by different manufacturers. All these fixtures are color-coded and have unique construction so that only the proper connector for each gas will fit in the outlet. Hospitals standardize one design of outlet to allow connectors to fit in different rooms. However, old and new buildings commonly have connectors that will not fit each other’s equipment even though they are both green oxygen hoses.
Each outlet and inlet needs to be regularly tested and approved by a technician certified by ASSE. This test can be done in a few minutes by plugging a rotameter into the outlet and logging the pressure and volume of the gas moving through the device.
The inspections can be done with the patient in the room and even when they are using one of the outlets simultaneously. Technicians can repair leaking or ill-fitting outlets and inlets without removing them from the wall. Typically, outlets and inlets come with a “front” and “back” structure that allows the most commonly worn parts to be replaced right in the patient's room in a few minutes.
Chapter 5
Hoses, Pigtails, and Connectors
There may be hoses that connect equipment to the wall that get reused. The hospital staff should inspect these lines to make sure they are not kinked or cracked. A kinked or cracked hose can lower system pressure or cause vacuum pumps to run excessively by sucking the air out of the room.
More common is the concern about the hoses in surgery areas. They can get bent, stepped on, and pinched by equipment. In the case of vacuum, they can also accumulate debris that reduces the system's efficiency in helping the surgical staff. The standard recommendation is that the booms and boom hoses get inspected or replaced every 18 months. Of course, each hose has its own color to indicate the kind of gas it carries and will have connectors at either end unique to the type of gas conveyed.
Connecting lines, or “pigtails”, from the gas cylinders to the manifold will usually be inspected and leak tested every six months. Since the cylinders containing the various gases run out and are replaced on a regular basis, these fittings and hoses get worn.
Most non-oxygen pigtails are stainless steel reinforced plastic to protect them from pinching and kinking among these bulky cylinders and in the tight spaces to connect and use wrenches to tighten fittings. The hoses are inspected for cracks and broken outside fibers. Replacement hoses must match the fittings for each kind of gas.
Conclusion
Medical gas systems in healthcare facilities can contain regulated drugs. The actual molecules are provided by outside vendors in a liquid or gaseous state. The delivery system is highly regulated, and the technologies used to deliver and monitor the administration of these drugs have multiple levels of supervision from the hospital, the industry, and the government.
Medical gas systems must be built by certified installers and then verified by a specially trained verifier before they can be used. Once the system is up and running, annual inspections make sure the patients and the staff are protected and served well by the system.
The information in this overview is believed to be accurate at the time of publication. Standards and rules are constantly evolving, and each facility may have special requirements that require accommodations.
The best procedure for any specific question about medical gas is to consult a certified expert like those at CHT. You can find detailed descriptions of these systems, their mechanisms, and the required safeguards in the publications and websites of:
- Center for Medicare and Medicaid Services
- The Joint Commission
- Occupational Safety and Health Administration
- American Society of Sanitary Engineers
- National Fire Protection Association
- American Society of Healthcare Engineering
CHT offers medical gas services to help you reach your compliance goals. To help you navigate through these challenges, we offer a free 30-minute discovery call.



