(Updated 1/2/2023)
Is your hospital prepared for another BIG emergency?
As the Plant Operations or Facility Manager, our commitment is to serve the community's health needs and do it economically while following the rules. The professional staff deftly handles everyday emergencies while we keep the lights on and the equipment working.
What happens to our facility if a disaster happens?
Hopefully, we can fall back on our plans.
The Centers for Medicare & Medicaid Services (CMS) are a leading authority in regulating healthcare requirements and providing materials guiding hospitals in emergencies. CMS’ emergency preparedness requirements went into effect in late 2016, were updated in 2019, and are due for another update soon.
What if there were a large-scale disaster near or around your facility? Think earthquake, flood, or terrorist attack that stops utilities for days or weeks. What would you need to have and need to do to keep the hospital running?
Basic Requirements for a Healthcare Organization
The first need is to keep the lights on. A facility should be able to easily do that with a built-in, regularly tested, backup generator.
What do you do if your 48 hours of emergency diesel fuel runs out? What about water; we take it for granted, but how long would your water tanks or reservoir last? Remember, if an attack shuts down your electricity, it also shuts down the water company.
6 Things to Consider as you Prepare an Emergency Preparedness Plan
1. Electricity - How do you provide and maintain power for two or more weeks while the infrastructure is being rebuilt?If the surrounding infrastructure loses power, you can lose phone service. How can information get in and out of the hospital? Do you have a satellite phone? How do outside vendors access your hospital, such as maintenance technicians or laundry providers? Are all of the hospital's vital systems correctly connected to emergency power?
2. Crowd Control - Who controls the crowds? Suppose the hospital is still standing while the surrounding community is experiencing a catastrophe. In that case, they will come flocking to you for not only medical care but also for food, water, and electricity. Who will you turn away? How will you enforce that policy?
3. Backup Medical Supplies - What backup supplies of medicines and disposables do you have on hand and in driving range, assuming there is gasoline for the ride?
4. Food - How many days of basic food do you have? How much should go to patients, staff, and the outside public?
5. Waste Management - How will you handle the waste stream? Soiled, bio waste and liquid waste if the sewers cannot take it.
6. Medical Gas Supply/Support What commitment can your medical gas suppliers make to you when asked about an emergency situation? Do you know their plans and priorities? How many medical consumables will your vendors promise to store locally and deliver in the case of a lengthy power and/or road shutdown?
Considering how much we take for granted in our civilized world, you can appreciate the agonizing decisions that hospitals worldwide have to make.
Many professional organizations have put together emergency plans that can be valuable guides for facilities to continue operating in the worst of times.
Notably:
California Emergency Physicians
Federal Emergency Management Agency
Centers for Medicare & Medicaid Services
Centers for Disease Control and Prevention
Conclusion
Your emergency preparedness plan will be unique to your location and conditions.
The last time a national emergency was declared, hospitals were the center for the community. It became evident what areas of operations had a plan, lacked a plan, or created response procedures on the go. The importance of an in-depth review of your hospital's emergency preparedness plan cannot be understated.
The organizations listed above and ASHE continue to assist members in staying CMS-compliant and preparing to serve their community under the most adverse conditions.
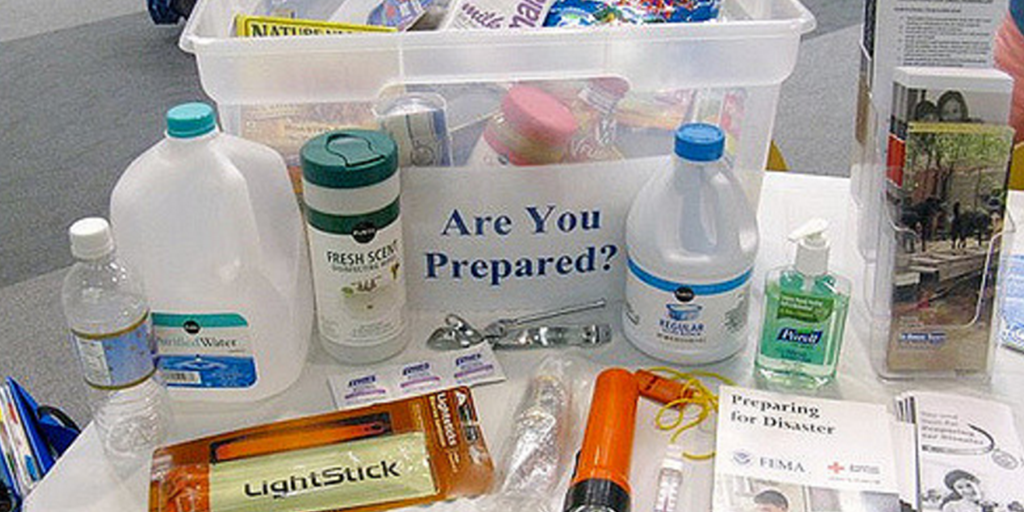
photo credit: Disaster kit




